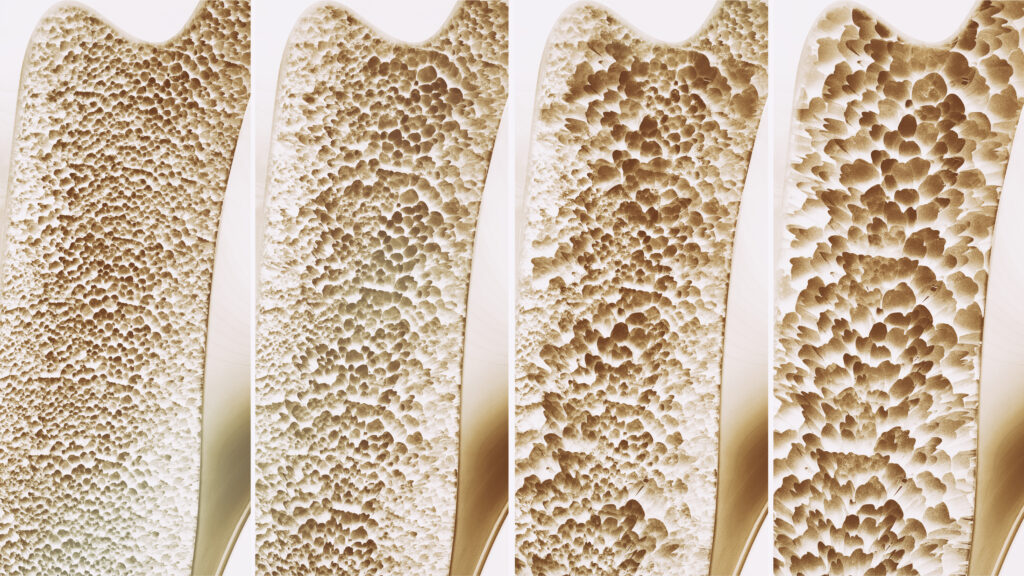
Osteoporosis is not just a condition associated with aging. It’s a silent threat that can have serious, even deadly consequences. Every year in the United States, approximately 300,000 hip fractures occur because of osteoporosis, making it one of the most common complications of this bone disease. About 75,000 Americans who experience a hip fracture die within the following year. Even for those who survive, the impact is profound. Another 75,000 individuals are forced to transition from the hospital to a nursing home, forfeiting their independence. For the remaining 150,000, regaining previous function becomes a monumental challenge, with only 15% able to walk across a room unaided six months after a hip fracture.
Osteoporosis is Treatable
Osteoporosis specialist Kacy Rogers, APRN, FNP-C, leads the Bone Health Clinic at OrthoIndy. “What makes osteoporosis particularly alarming is that it’s not only prevalent but also often goes undiagnosed and untreated,” Rogers said. Despite its treatable nature, a staggering 84% of patients with osteoporotic fractures do not receive the necessary medical attention. This negligence leads to nearly 2 million broken bones each year, with half of repeat fractures being entirely avoidable through cost-effective treatments.
Osteoporosis is Common
The statistics paint a clear picture: osteoporosis is a serious, common, and costly health issue. One in two women over the age of 50 will experience a bone fracture due to osteoporosis, along with one in four men of the same age group. The economic burden is substantial, with osteoporosis-related fractures costing an estimated $52 billion in 2018 alone. Alarmingly, this figure is projected to rise to $95 billion by 2040, with over 3.2 million fractures annually attributed to osteoporosis.
How is Osteoporosis Diagnosed?
So, how can individuals protect themselves from this silent threat? “Understanding the importance of diagnosis is key,” Rogers noted. There are three primary methods for diagnosing osteoporosis:
- Bone Density Test: Also known as dual-energy X-ray absorptiometry (DXA), this test measures bone mineral density, often represented by a T-score. It’s the most common method for diagnosing osteoporosis.
- Fracture: If you’re over 50 and have experienced a fracture in certain areas like the spine, hip, wrist, shoulder, or pelvis, it’s likely you have osteoporosis, regardless of your T-score.
- FRAX: This fracture risk calculator assesses the likelihood of different types of fractures occurring over the next decade. If your probability of major osteoporotic fracture or hip fracture meets certain thresholds, a diagnosis of osteoporosis can be made.
Moreover, certain demographics should prioritize bone density testing, including women over 65, men over 70, and anyone over 50 who has experienced a bone fracture. Additionally, individuals aged 50-64 with specific risk factors, such as family history, frequent falls, or certain medical conditions, should also undergo testing.
Recognizing risk factors and taking proactive measures can significantly reduce the impact of osteoporosis. Whether it’s ensuring an adequate intake of calcium and vitamin D, maintaining a healthy lifestyle, or seeking medical advice regarding medications that may impact bone health, early intervention is crucial.
Osteoporosis is not a condition to be underestimated. Its consequences are severe, affecting millions of lives and costing billions of dollars annually. By prioritizing early detection, intervention, and preventive measures, individuals can safeguard themselves against the silent threat of osteoporosis and enjoy a higher quality of life for years to come.