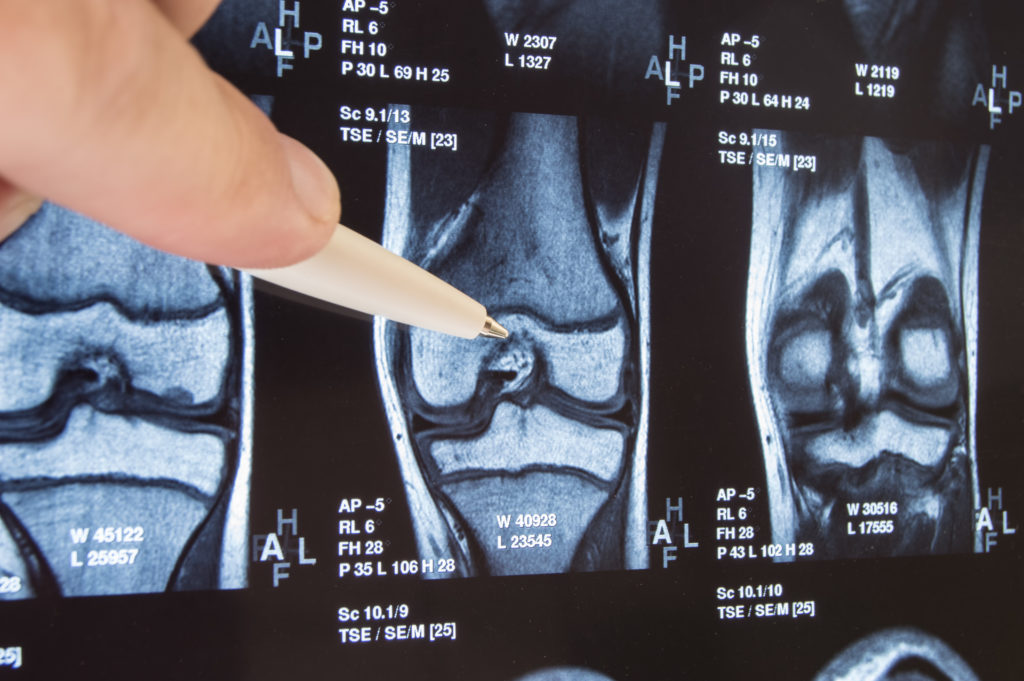
OrthoIndy cartilage restoration specialist, Dr. Jack Farr explains recurrent patellar (knee cap) dislocations.
After the first patellar (knee cap) dislocation, a percentage of patients will experience another dislocation(s). The probability of this occurring is related to certain risks factors that can be identified with X-rays and MRI. The most commonly cited risk factors are: high riding patella, excessive lateral position of the attachment of the patellar tendon attachment to the tibia, “knock-knees”, residual excessive looseness of the medial patellofemoral ligament or poor trochlear groove shape.
What is a high riding patella?
Patellar alta is an anatomic term, which means the patella rides higher (in the direction of the hip) above the knee joint line than “normal.” These measurements of patellar height are expressed as a ratio. The normal range is between 0.8 and 1.2. With patellar alta, for any give knee flexion angle, the patella enters the femoral groove later and thus the stability of the trochlear groove occurs later. The femoral trochlear groove aids in guiding the patella and becomes deeper (more guidance) with greater flexion. Thus, those patients with patellar alta, do not have as much groove patellar guidance, making it easier for the patella to escape/dislocate.
What is excessive lateral position of the patellar tendon attachment to the tibia?
The quadriceps muscle pulls the leg from flexion to extension acting through the tendon of the quadriceps, which attaches to the patella, which attaches to the leg bone (tibia) through the patellar tendon. If these attachments are close to a straight line, the patella is pulled smoothly within the central region of the trochlear groove. If the attachments are not near a straight line, the patella would be pulled to one side or another. In patients, this altered position (some term it “malalignment”) of the patellar tendon attachment to the tibia (tibial tuberosity/tubercle), will result in forces acting on the patella to pull it out of the trochlear groove to a variable extent.
The position of the tuberosity can be measured on MRI or CT and is calculated from a femoral reference point (trochlear groove, TG) or the tibia (posterior cruciate ligament, PCL). These studies measure how far lateral (toward the outside of the knee) the tibial tuberosity/tubercle (TT) is from the reference point. The TT (if no prior surgery) is always lateral in patients. Several studies have measured these distances in patients with and without patellar dislocations. The reference number for patients without patellar dislocations is 10-13 mm for the TT to TG distance. Those with recurrent dislocations have greater probability of having lateral distances. Patellofemoral (PF) surgeons consider the distances to be frankly abnormal if the TT-TG is above 20 mm or if the TT-PCL is above 24 mm.
What is “knock knees?”
With neutral limb alignment, when a patient stands, the ankles and knees touch. With “bowed-knees”, the ankles touch, but there is a space between the knees: termed varus knees. In those with “knock-knees” when the knees touch, the ankles are apart: termed valgus knees. As the ankles define the distal aspect of the tibia, this means the tibia is angled outward with respect to the femur. The lateral position of the tibia also causes the tibial tuberosity/tubercle to be located more laterally, and thus have a similar effect as a TT located excessively lateral as above. Both conditions may exist together or one can be elevated and the other within normal limits.
What is residual excessive looseness of the medial patelloFemoral ligament (MPFL)?
The medial patellofemoral ligament (MPFL) runs from the inside (medial) aspect of the femur at the knee to the patella. It does not actively pull the patella into the groove, but rather keeps it from exiting or dislocating from the groove. This acts much the same as a dog leash: it does not restrict the dog from movement until the dog gets to the end of the leash at which point the dog can go no further. With a first time patellar dislocation, this ligament is injured/torn/sprained. In some cases, the ligament heals with good tissue strength and normal length. When the ligament fails to heal, heals with wispy scar tissue or heals in a lengthened state, it will not be able to stop the patella from dislocating.
What does poor trochlear groove shape mean?
The trochlea groove can be thought of as a “V” shape pulley that aids in guiding the patella as the knees flex. If the natural “V” shape is shallow or replaced by a flat or domes trochlea this abnornal shape is termed trochlear dysplasia. Just as a flat pulley would not keep a rope in place, a dysplastic trochlea makes it easier for the patella to escape/dislocate.
To make an appointment with Dr. Farr please call 317.884.5163 or learn more about cartilage restoration.
Schedule an appointment
Your well-being is important to us. Click the button below or call us to schedule an appointment with one of our orthopedic specialists. If your injury or condition is recent, you can walk right into one of our OrthoIndy Urgent Care locations for immediate care. For rehabilitation and physical therapy, no referral is needed to see one of our physical therapists.