Dr. Jack Farr, OrthoIndy cartilage restoration surgeon, answers common questions about cartilage restoration.
What is knee cartilage restoration?
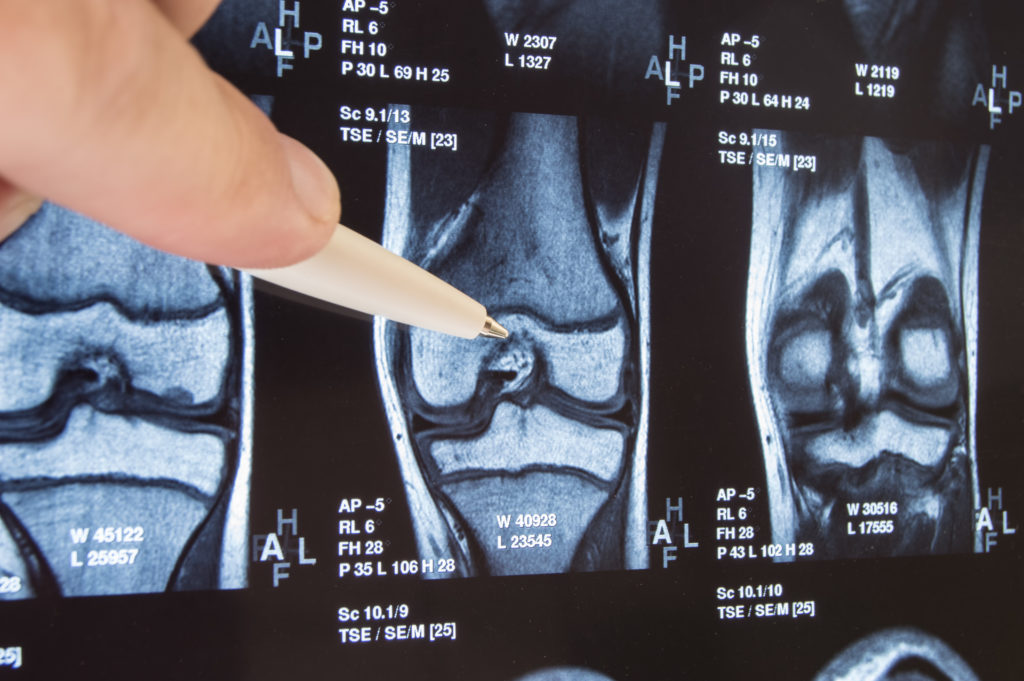
A. Cartilage restoration is a term often used interchangeably with cartilage repair. For example, “Bill tore his cartilage playing basketball and will need it repaired.” In this case, it is the meniscus cartilage. Repair, in this sense, means to aid the tissue to return to its original function. Unfortunately, only about 10% of meniscal cartilages are amenable to repair and articular cartilage does not have a natural healing pathway. The consequential defects may have new tissue implanted to restore function. This is cartilage restoration.
Who is the ideal patient for cartilage restoration?
A. Restoring a meniscus or articular cartilage defect depends on many factors in addition to the defect alone. Typically, the patient needs to be fully rehabilitated, have near normal limb alignment, a stable knee and a body mass index of less than 35. Many insurance companies allow cartilage restoration between the ages of 15 and 50.
What are the surgical options for cartilage restoration?
A. Marrow Stimulation.
This repair tissue develops from cells from the bone marrow. They migrate to the injured cartilage area through small holes (made by a ”pick” or drill) in the bone. This can be thought of as repairing “potholes” in a road. It may not last as long as a normal road, but it is often successful in eliminating symptoms in many patients.
Osteochondral Autograft
This technique is similar to a hair-plug transfer. The surgeon removes a small plug section of the patient’s own cartilage along with an attached underlying bone plug. These donor plugs are obtained from an area of the knee, which does not participate in high loading. This bone and cartilage plug graft is then transferred to the defect, which has been prepared into a socket. Obviously, only so much donor tissue is available, so this technique is used primarily for small cartilage defects.
Autologous Chondrocyte Implatation (ACI or Carticel)
This is one of the pioneering techniques in cartilage restoration and is performed in two stages. A small amount of the patient’s own articular cartilage is harvested. Then, through cell culturing techniques, the cell number is increased from a few hundred thousand to more than 10 million cells. These cultured cells are then re-implanted into the knee cartilage defect under a watertight biologic patch (patient’s own periosteum) placed over the defect. The cells then gradually form hyaline-like cartilage to resurface larger cartilage defects.
Osteochondral Allograft
For large defects of cartilage loss, surgeons can implant a freshly donated cadaver cartilage and bone plug or shell that may allow restoration of joint function. The tissue is maintained viable with cooled culturing media while the donor is tested for possible disease transmission. It is necessary to size match the graft to the patient, which further complicates availability.
Juvenile Particulated Articular Cartilage (DeNovo NT)
Dr. Yao and I published the first short series of patients in the journal “Cartilage” in 2011, which showed young donor cartilage when minced into small cubes can grow new cartilage in a defect. A more extensive series of similar patients also revealed patient improvements as reported in the American Journal of Sports Medicine, April 2014. Since starting in 2007, over 6000 US patients have been treated with DeNovo NT.
Meniscial Allograft Transplantation
With meniscal transplantation, a sized-matched cadaver donor meniscus is transplanted into the site of the original meniscus. Unlike soft tissue organ transplantation, this procedure does not require patients to be on medications to prevent rejection. I share a patent for one of the instrumentation systems that assist surgeons in performing the procedure.
What is the benefit of cartilage restoration surgery?
A. The number one is goal is to decrease pain and improve function. It is our hope that cartilage restoration may delay joint replacement surgery, especially in young patients.
What is rehab for cartilage restoration surgery patients?
A. Most cartilage procedures require a period of limited weight-bearing to allow early healing. The range of motion is encouraged from the start. Most patients are able to perform a home exercise program often with the oversight of a physical therapist. Depending on the type of restoration, the improvements may be seen as early as a few months (osteochondral autograft) to many months for larger lesions treated with cell therapy (ACI).
Is there anything else you would like to add?
A. At the OrthoIndy Cartilage Restoration Center of Indiana, we not only offer the above standard treatments but continue to investigate new options. As a result, we participate in various new projects. Up to date information may be found at www.CartilageRestoration.org and www.clinicaltrials.gov. To make an appointment with Dr. Farr please call 317.884.5163 or learn more about cartilage restoration at OrthoIndy.
Schedule an appointment
Your well-being is important to us. Click the button below or call us to schedule an appointment with one of our orthopedic specialists. If your injury or condition is recent, you can walk right into one of our OrthoIndy Urgent Care locations for immediate care. For rehabilitation and physical therapy, no referral is needed to see one of our physical therapists.